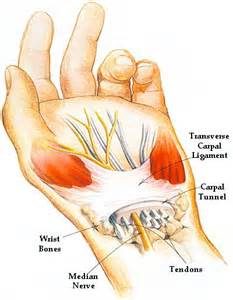
 Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis.
Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis.
Proper treatment usually relieves the tingling and numbness and restores wrist and hand function. It is worth noting that carpal tunnel syndrome is often misdiagnosed and the main site of median nerve compression can be occurring up at neck and shoulder level. Often by freeing up neck and shoulders muscles and surrounding joints with physio as well as working out muscles down along the arm through which the median nerve penetrates, and loosening and stretching the wrist structures, much relief, often total relief can often be achieved.
Symptoms
Syndrome symptoms usually start gradually.
Numbness: The first symptoms are usually tingling or numbness usually in the thumb, index and middle or ring fingers, but not your little finger. The sensation may travel from your wrist up your arm. These symptoms often occur while holding a steering wheel, phone or newspaper. The sensation may wake you from your sleep.
Weakness: You may experience weakness in your hand and a tendency to drop objects. This may be due to the numbness in your hand or weakness of the thumb’s pinching muscles, which are also controlled by the median nerve.
Carpal Tunnel Risk factors
A number of risk factors have been associated with carpal tunnel syndrome. Although they may not directly be the cause , they may increase your chances of developing or aggravating median nerve damage.
These include:
Anatomic factors: wrist fracture, dislocation, or arthritis that deforms the small bones in the wrist, can alter the space within the carpal tunnel and put pressure on the median nerve.
Sex: It is generally more common in women. This may be because the carpal tunnel area is relatively smaller in women than in men.
Nerve-damaging conditions: Some chronic illnesses, such as diabetes, increase your risk of nerve damage.
Inflammatory conditions: Illnesses that are characterized by inflammation, such as rheumatoid arthritis, can affect the lining around the tendons in your wrist and put pressure on your median nerve.
Obesity : Being obese is a significant risk factor for carpal tunnel syndrome.
Alterations in the balance of body fluids. Fluid retention may increase the pressure within your carpal tunnel, irritating the median nerve. This is common during pregnancy and menopause. Carpal tunnel syndrome associated with pregnancy generally resolves on its own after pregnancy.
Carpal Tunnel Diagnosis
History of symptoms, Physical examination. Nerve tension tests.
X-ray. Some doctors recommend an X-ray of the affected wrist to exclude other causes of wrist pain, such as arthritis or a fracture.
Electromyogram. This test measures the tiny electrical discharges produced in muscles. During this test, your doctor inserts a thin-needle electrode into specific muscles to evaluate the electrical activity when muscles contract and rest. This test can identify muscle damage and also may rule out other conditions.
Nerve conduction study. In a variation of electromyography, two electrodes are taped to your skin. A small shock is passed through the median nerve to see if electrical impulses are slowed in the carpal tunnel. This test may be used to diagnose your condition and rule out other conditions.
Treatment
If the condition is diagnosed early, nonsurgical methods may help improve carpal tunnel syndrome. Physical therapy by a practitioner experienced in this area can be very effective. This would most like involve deep tissue work, osteopathic manipulations, electroacupuncture and postural correction exercises, and nerve glide exercises as the condition improves. Other treatment options include wrist splinting, taking more frequent breaks to rest your hands, avoiding activities that worsen symptoms, medications(Nonsteroidal anti-inflammatory drugs) icing, rest etc. Surgery is also an option but is a last resort.
For treatment of this condition contact us on 0867700191
For more information see this video
 Muscles are made up of fibers that your nerves control. Muscle twitching is caused by minor muscle contraction in the area, or uncontrollable twitching of a muscle group that is served by a single motor nerve fiber. Stimulation or damage to a nerve may cause your muscle fibers to twitch. Most muscle twitches are minor and aren’t usually a cause for concern. Some are common and normal. Others are signs of a nervous system disorder.
Muscles are made up of fibers that your nerves control. Muscle twitching is caused by minor muscle contraction in the area, or uncontrollable twitching of a muscle group that is served by a single motor nerve fiber. Stimulation or damage to a nerve may cause your muscle fibers to twitch. Most muscle twitches are minor and aren’t usually a cause for concern. Some are common and normal. Others are signs of a nervous system disorder.
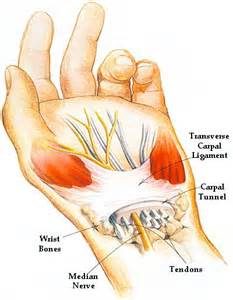 Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis.
Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis. When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time.
When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time. One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
 cartilage can be damaged by injury or normal wear and tear.
cartilage can be damaged by injury or normal wear and tear.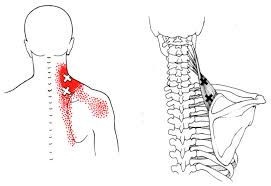

 Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
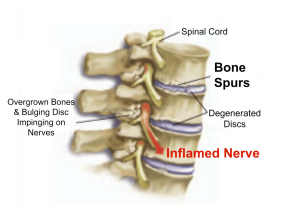 Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons .
Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons .